Medtransic Announces MAGENTIC – A New AI-Driven Solution to Combat Healthcare Revenue Cycle Challenges
Medtransic unveils advanced AI tools to help healthcare providers overcome escalating administrative costs and improve the revenue cycle in 2026.
United States, 4th Feb 2026 – The United States healthcare system continues to grapple with the ever-growing issue of administrative waste, now estimated to cost the industry over $600 billion annually. This staggering figure underscores the urgent need for innovation in medical practices, especially as the pressures from administrative tasks, including billing and claims processing, continue to escalate. In 2026, these challenges have become existential threats for many providers.
While the clinical side of healthcare has rapidly advanced with new technologies, the financial infrastructure remains mired in outdated processes. Insurance payers have increasingly turned to sophisticated AI-powered “denial engines” that automatically reject claims for even minor errors, often before a human can intervene. Providers find themselves fighting this advanced, automated system with outdated manual processes. To survive, they must stop viewing billing as merely a back-office task and recognize it as a critical technological defense.
The Decline of the “Clean Claim”
For many years, a healthy medical practice was defined by maintaining a 95% clean claim rate, with minimal claim rejections and denials. However, recent data from the Medical Group Management Association (MGMA) reveals that this number is no longer achievable for most practices. Denial rates for initial claims have surged to nearly 15%, significantly impacting practice revenue. This trend can be attributed to “Payer Policy Drift,” the constant and often unannounced changes in billing rules and medical necessity guidelines that trigger automatic claim rejections.
Every denied claim incurs a “rework tax,” where practices must spend valuable time and resources appealing claims. Premier, Inc. reports that, on average, it costs $57 to appeal a single denied claim. In specialties with high complexity, the cost of an appeal can climb to over $180 per claim. For high-volume surgical centers or multi-specialty groups, these “minor” costs can add up quickly, draining hundreds of thousands of dollars in lost income each year.
The Hidden Human Cost of Administrative Burden
The financial toll of this administrative burden extends far beyond monetary losses. The United States is also facing a national crisis of physician burnout, with a staggering 93% of physicians citing administrative hurdles, particularly related to prior authorizations, as the primary cause of delayed patient care.
“The system is fundamentally broken,” said Nasar Haq, founder of Medtransic. “Practices are exhausted. We’re seeing brilliant clinicians penalized for the complexity of the care they provide because their billing systems are stuck in 2015. You cannot fight 2026-level automated denials with more manual labor. The math simply doesn’t work anymore. Every hour a nurse spends on hold with a payer is an hour stolen from a patient.”
This “Administrative Tax” is taking its toll on the provider-patient relationship, shifting the focus from delivering care to dealing with financial and bureaucratic hurdles. For many healthcare providers, the administrative challenges are becoming an existential threat, threatening the viability of their practices and quality of patient care.
A Shift from Reactive to Proactive Revenue Cycle Management
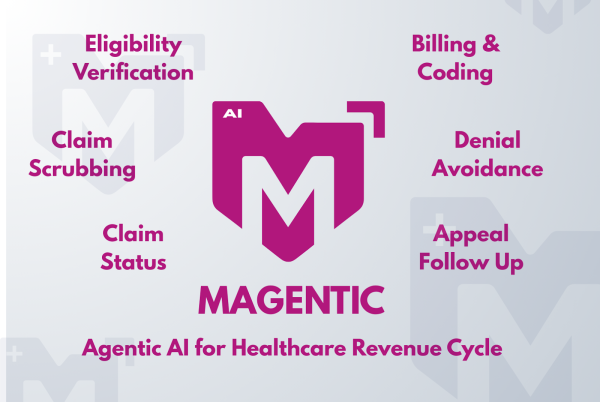
To survive, practices must stop relying on the traditional “Submit, Deny, Appeal” model of revenue cycle management (RCM). This reactive approach is no longer sustainable and leaves providers perpetually on the defensive. The solution, according to Medtransic, lies in shifting to a “Pre-active” approach by leveraging advanced AI-powered systems that serve as proactive “Agentic AI” digital teammates.
Unlike basic robotic process automation (RPA), Agentic systems are designed to operate with intentionality and planning. These AI tools proactively navigate payer portals to verify insurance eligibility and simulate payer logic to identify potential denial triggers before a claim is even submitted. This allows practices to address issues before they become denials, drastically reducing administrative overhead.
“Our goal at Medtransic is to make the financial side of medicine invisible,” Haq explained. “We use autonomous agents to handle the high-volume, repetitive tasks, such as status checks, technical scrubbing, and eligibility, so human experts can focus on cases that require real expertise. We’re not just filing papers; we’re building a technological defense for the practice. It’s about giving the provider the upper hand in the AI arms race.”
Enhancing Patient Experience Through Financial Transparency
In 2026, one of the greatest sources of patient dissatisfaction is unexpected medical bills that come as a surprise after procedures. This financial “sticker shock” often arises from misunderstandings about insurance coverage at the front desk.
By using Agentic AI to automate the front-end of the revenue cycle, practices can offer accurate and timely “Good Faith Estimates” to patients. This real-time transparency fosters trust between providers and patients, as patients are better informed about their financial responsibilities from the start. With more accurate estimates, practices can confidently collect co-pays and deductibles, reducing the need for costly “small-balance” collections later on.
The Future of Healthcare Revenue Cycle Management
As the healthcare landscape evolves in 2026, the practices that will thrive are those that recognize revenue cycle management (RCM) as a technology-driven defense, not just a back-office chore. Outdated, manual billing departments are becoming a serious financial liability, hindering long-term growth. By embracing AI-driven automation, practices can reclaim their financial health and, in turn, their focus on patient care.
The shift from reactive to proactive RCM isn’t just about increasing margins, it’s about preserving the sanctity of the doctor-patient relationship and ensuring the future of independent medicine. In the current “AI Arms Race,” the only way to win is to stop playing defense and start automating the offense.
About Medtransic
Medtransic is a cutting-edge healthcare technology company dedicated to transforming the revenue cycle management (RCM) process for healthcare providers. By leveraging advanced AI and autonomous digital agents, Medtransic aims to streamline billing, reduce administrative waste, and improve the financial health of medical practices. The company’s solutions allow providers to focus more on patient care by automating repetitive tasks and addressing denial risks before they occur. Medtransic’s mission is to help healthcare providers navigate the complexities of the modern healthcare landscape with innovative, technology-driven solutions.
Phone: 1(888) 777 0860
Website: medtransic.com
LinkedIn
Facebook
Company Details
Organization: Medtransic
Contact Person: Jim Hayes
Website: http://medtransic.com
Email: Send Email
Country: United States
Release Id: 04022640999
